Menopause and sleep: The struggle is real (and so are these solutions)
If only you could sleep in the fridge, then menopause wouldn’t be a problem.
There, snuggled up next to the baloney, head resting on a cool heirloom tomato, you’d finally be able to sink into a cool, temperature-controlled slumber.
For many people, the above fantasy, no doubt, sounds… bizarre.
If you’re nearing menopause, however, we’re guessing you can relate.
Though we can’t offer any advice that will erase every single symptom, we can help ensure this rite of passage doesn’t wreck your sleep.
In this article, we’ll explain why sleep becomes so elusive around menopause (hint: it’s not all about hormones).
Plus, we’ll give you (or your clients) five ways to manage symptoms—and sleep easier.
Worry not: Cooler, more restful nights are in your future.
++++
The real reason menopause affects sleep
Menopause is marked by a full year without a menstrual period.
Long before your final period, during perimenopause, levels of estrogen, progesterone, luteinizing hormone (LH), and follicle-stimulating hormone (FSH) fluctuate. This can affect your sleep wake cycle (a.k.a. your circadian rhythm), body temperature regulation, mood, and sleep quality, as this chart shows.1,2,3
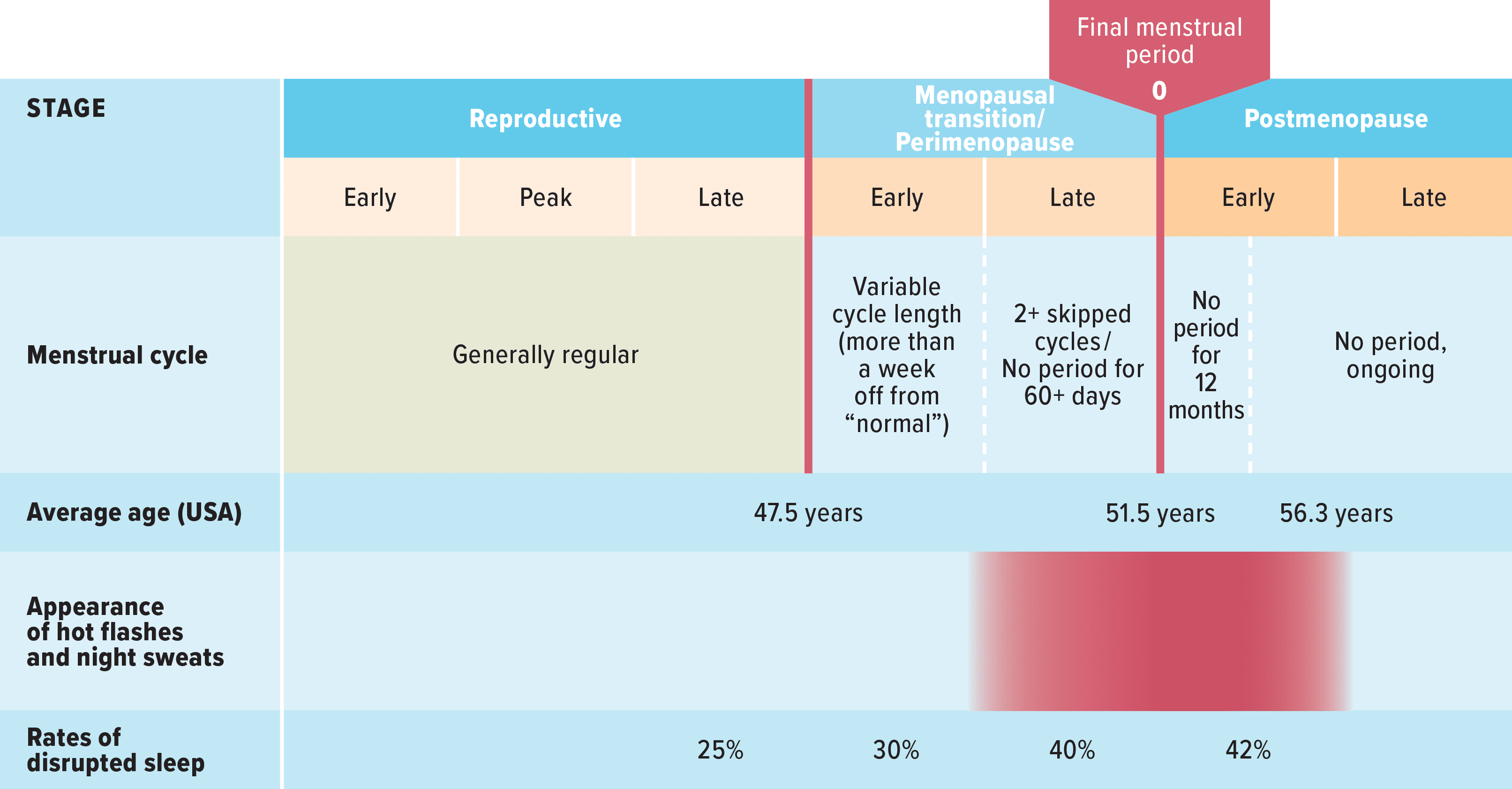
Once you reach menopause, levels of estrogen and progesterone will typically be more stable—and quite low. A few years after you’ve waved a final goodbye to your monthlies, thankfully, your symptoms and sleep issues may dissipate. (No wonder the menopausal transition is so frustrating!)
Despite all this, it’s important to know:
Sleep disruptions are caused by many different factors, not just hormones.
Many biological, psychological, and social factors can affect sleep.
For example, you might also experience changes in:
 Metabolism: As you approach menopause, abdominal fat tends to accumulate—which increases your risk of insulin resistance.4
Metabolism: As you approach menopause, abdominal fat tends to accumulate—which increases your risk of insulin resistance.4
This, in turn, can change how often you need to go to the bathroom, or how thirsty you feel.5 (Meaning: You find yourself making more trips to the bathroom at night, or to the kitchen for a glass of water.)
 Mood and mental health: Almost like a second puberty, you may discover new depths of hair-trigger rage, or a sadness you haven’t felt since you were 13 and your mom wouldn’t let you sleep at Janey’s house on a school night.
Mood and mental health: Almost like a second puberty, you may discover new depths of hair-trigger rage, or a sadness you haven’t felt since you were 13 and your mom wouldn’t let you sleep at Janey’s house on a school night.
These mood changes are thought to be connected to sleep disruptions.6
 Roles, relationships, and general health and aging: The onset of menopause may go along with other big life changes:
Roles, relationships, and general health and aging: The onset of menopause may go along with other big life changes:
- Jobs or financial status (losing a job, retiring, paying for kids’ college, supporting a relative)
- Relationships (deaths of parents or friends, divorce, estrangement)
- Overall health (due to aging, the accumulation of poor health habits, or just bad luck)
- Sex drive (from lack of desire, vaginal dryness, fatigue)
- Familial responsibilities (your nearing-adulthood kids might not need you as much, but your aging parents might need you more)
- Body image (aka “who the heck is that person in the mirror?!”)
- Identity (struggling with who you are, or the fear of aging and mortality)
No wonder you feel as if you can’t power down at night.
(And just when you do, there’s your bladder calling again.)
5 ways to improve sleep
Make each night more restful by experimenting with the following solutions.
1. Prepare for those night sweats.
The following three ideas are… three ideas. We could have listed dozens.
We welcome you to experiment with what we’re suggesting here, as well as try different strategies. If the lady at the crystal store said that giant amethyst will help you sleep better—and it consistently works for you—onwards!
 Keep a spare set of PJs or a towel beside the bed. This way, when you wake up soaked, you won’t have to search for something clean and dry.
Keep a spare set of PJs or a towel beside the bed. This way, when you wake up soaked, you won’t have to search for something clean and dry.
 Sleep with a fan. The cool air will minimize the chances of overheating. Plus, it doubles as a white noise machine if your partner’s (or dog’s) snoring occasionally wakes you up.
Sleep with a fan. The cool air will minimize the chances of overheating. Plus, it doubles as a white noise machine if your partner’s (or dog’s) snoring occasionally wakes you up.
 If you have the financial means, try cooling sheets, pads, and pillows. These products range from breathable, sweat-wicking fabrics to full-on electric covers and pads that allow you to set your preferred sleeping temperature.
If you have the financial means, try cooling sheets, pads, and pillows. These products range from breathable, sweat-wicking fabrics to full-on electric covers and pads that allow you to set your preferred sleeping temperature.
While the above tools might not completely vanish sleep problems, they can minimize one of the more disruptive symptoms, and give you—or your client—a sense of control.
2. Reframe your thoughts about sleep loss.
Night sweats can create a vicious circle.
They wake you one night. You feel tired the next day. The following night, you think, “I NEED to sleep.” But, no, you’re up and sweating again.
Eventually the sweating might stop, but you’re still… awake.
What gives?
When you layer anxiety about sleep overtop of existing sleep disruptions, you lose rest not just because of night sweats, but also because of the catastrophic thoughts you have about how your sleep loss is somehow going to make you lose your job.
To turn this around, steal a strategy from cognitive behavioral therapy (CBT), which has been shown to be extremely effective for sleep anxiety.
Write down the thoughts or beliefs that come up when you can’t sleep.
For example:
- I’ll never sleep well again.
- I can’t work out / think clearly / take care of everyone because I’m so tired.
- My bad sleep is going to cause me to get some terrible illness, like cancer or heart disease.
Notice how worried thoughts tend to:
- Use absolutes (like “always” or “never”)
- Predict the future (even though you’re not a licensed fortune-teller)
- See things as “all-or-nothing” (“If I don’t sleep well, I can’t do ANYTHING.”)
Now, reframe those beliefs using a realistic, compassionate perspective.
For example:
- I might lose sleep occasionally, but other nights will probably be okay.
- I’m not feeling my best, but I can do some exercise / work and maybe find a few moments of peace in my day.
- Sleep is just one aspect of good health. If I don’t sleep well, I can still make sure I eat nutritious foods, drink enough water, and get outside for a few deep breaths.
By training yourself to reframe your thoughts about sleep, you can minimize how much you worry about sleep, allowing you to, well, sleep.
3. Design better days for better nights.
Restful sleep has as much to do with what you do during the day as it does with what you do at night.
When your days are filled with relentless stress—particularly if that stress feels isolating, purposeless, and unending—it’s understandable if your body’s still buzzing when it’s time to turn off.
This is especially true around perimenopause, when loopy hormones can make you extra sensitive to stress.
While you can’t always prevent stressful moments like the dishwasher breaking down right after you’ve made your cheesy macaroni casserole, you can improve how you recover from these unwanted life events.
Think of yourself as a jug (okay, not glamorous… but bear with us):
Stress drains the jug, and recovery fills it back up.
The image below offers several ways to recover, and there’s more in this article too: Secrets for using stress to build you up—instead of break you down. 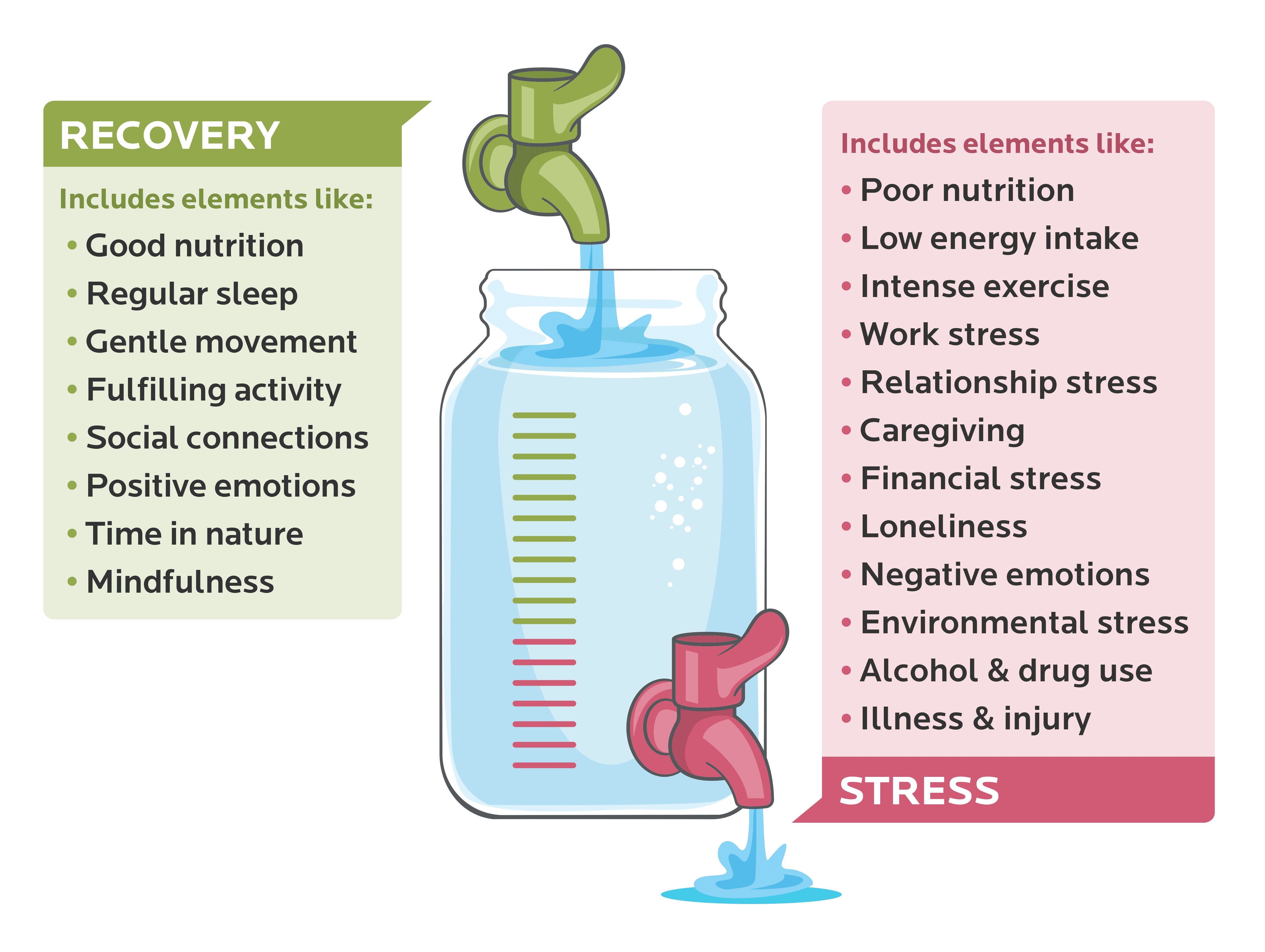
Try to fill your jug, at least as much as you drain it, by punctuating your days with moments of:
- Rest (like a 10-minute guided meditation after an intense meeting)
- Joy (grabbing a coffee with your friend who always makes you laugh)
- Self-kindness (protecting your time to take care of yourself)
When you do that, you’re less likely to lie awake because you haven’t stopped all day and this resting thing feels so foreign (and you’re dreading the next day).
Instead, you’ll be reminiscing about the good conversation you had with a friend, and looking forward to that tai chi class you registered for at your local community center.
(Cool fact: Tai chi—as well as yoga, meditation, and other relaxation practices—aren’t just good for your overall health and fitness. They also can alleviate symptoms of menopause, including hot flashes, mood swings, and sleep loss.7)
Menopause Rx: Talk to your doctor about these sleep-management tools
If menopause-related symptoms are severe, persistent, and overwhelming, talk to your doctor about whether you’re a good fit for…
Menopausal hormone therapy (MHT): MHT can improve sleep quality, decrease the time it takes to fall asleep, and reduce the number of nighttime awakenings.6,8,9 Caution: It can also raise disease risk for some women, so a conversation with your doctor is important.10
Antidepressants: If sleep issues are primarily due to persistent mood issues like anxiety and depression (and not night sweats), antidepressants can help.11 When treating sleep, these medications are usually recommended in combination with CBT-I, a form of cognitive behavioral therapy specifically used to improve sleep.
Prolonged/slow release melatonin: Talk to your doctor to see if you’re a good candidate for melatonin—a hormone you naturally produce in your brain that regulates your sleep-wake cycle. In research, two milligrams has been shown to be effective.11
4. Bring some self-compassion and common humanity to your situation.
Self-compassion can activate your calming nervous system and improve sleep.12 The elements include:
- Mindfulness: Notice what you’re feeling. (For example, validating for yourself, ‘Hey, retiring from a career or dealing with an aging parent, is stressful.’)
- Common humanity: Appreciate how universal your experience is. You’re not alone, and so many women are going through this too. Imagine all those women, just like you, staring at the ceiling. Send them some imaginary kindness, and mentally reassure them that they’ll be okay too.
- Self-kindness: Speak to and treat yourself with care. Even if you’ve snapped at your partner way too many times this morning (“After 20 years of marriage, STILL with the toilet seat?!”), you’re not a monster. You’re just a human, trying to do your best. Ask yourself what you need to care for yourself, and try to prioritize it.
Admittedly, self-compassion won’t change that you can’t wear wool anymore. Or that everyone’s getting older.
But it can change how you experience your situation, possibly even making the experience of menopause more unifying, cathartic, and empowering.
5. Notice your strengths and superpowers.
During peri- and post-menopause, a lot can feel out of your control—on your worst days, like a slippery slope towards doom.
Transition periods can trigger these feelings: The old way is lost, but the new path isn’t visible yet. Meanwhile, you’re tangled in branches and fighting off angry squirrels in the dark woods of the in-between.
So, shine a light on the good.
If you’re lying awake at night worrying about how much you’re going to miss your kid who’s going away to college: You must be someone who cares deeply about your relationships.
If you’re tossing and turning about a presentation you have to give in the morning: You must be someone with a strong attention to detail.
If you’re wondering how you’re going to make a casserole for a grieving friend, work, volunteer as a crossing guard, and visit your dad: You must be someone that other people depend on.
Whatever you’re struggling with, there’s a flipside: That side reveals your values, your strengths, and your unique superpowers.
So, when you’re having a hard time, ask yourself:
‘Why does this matter to me?’
Let the answer point you to what’s special about YOU.
And celebrate it.
Because if anything, menopause is a victory. You’ve made it this far. And the next adventure is waiting.
References
Click here to view the information sources referenced in this article.
If you’re a health and fitness coach…
Learning how to help clients manage stress, build resilience, and optimize sleep and recovery can be deeply transformative—for both of you.
It helps clients get “unstuck” and makes everything else easier—whether they want to eat better, move more, lose weight, or reclaim their health.
And for coaches: It gives you a rarified skill that will set you apart as an elite change maker.
The brand-new PN Level 1 Sleep, Stress Management, and Recovery Coaching Certification will show you how.
Want to know more?
The post Menopause and sleep: The struggle is real (and so are these solutions) appeared first on Precision Nutrition.

Nenhum comentário