PCOS: 3 evidence-based strategies that really work.
Reviewed by Stephanie Paver, MS, RD
What is PCOS | Causes | Symptoms | PCOS Diet | Treatment | Weight Loss | For Coaches
Acne, hair in weird places, weight gain, wonky periods, and fertility struggles.
Those are just some of the symptoms of polycystic ovary syndrome (PCOS), a hormonal problem that affects up to 20 percent of women worldwide.1, 2
Because of its varied symptoms along with the lack of a clear diagnostic test, some women must wait years—and see multiple health professionals—before they get an accurate diagnosis.3
Even with good advice, women with PCOS may struggle to do what they know is good for them:
 If fatigue is an issue, exercise can feel as appealing as hauling garbage on a hot day.
If fatigue is an issue, exercise can feel as appealing as hauling garbage on a hot day.
 If sleep is elusive, appetite might intensify, making processed foods seem all the more irresistible.
If sleep is elusive, appetite might intensify, making processed foods seem all the more irresistible.
 If mental health is suffering, everything might seem harder.
If mental health is suffering, everything might seem harder.
Also frustrating: Trying to find consistent, evidence-based PCOS advice on the Internet. Seriously. Ugh.
That’s why we wrote this article—so coaches and people with PCOS can find trusted advice that actually works.
++++
What is polycystic ovary syndrome (PCOS)?
Physicians diagnose PCOS when someone exhibits at least two of the following:
✓ Irregular periods: They may be shorter than 21 days, longer than 35 days, or completely absent.
✓ “Cysts” in the ovaries: Confirmed by an ultrasound, these growths aren’t true cysts, but rather a build-up of egg follicles.
✓ High androgen levels, like testosterone: This is confirmed by a blood test or visible signs like facial hair, acne, or male pattern baldness.
Though not a diagnostic criteria, high insulin levels and a reduced ability to tolerate carbohydrates are also common.
Biology lesson: The PCOS hormonal cascade
PCOS likely originates in the hypothalamus, a small region in the brain which—among other things—is in charge of regulating hormones.
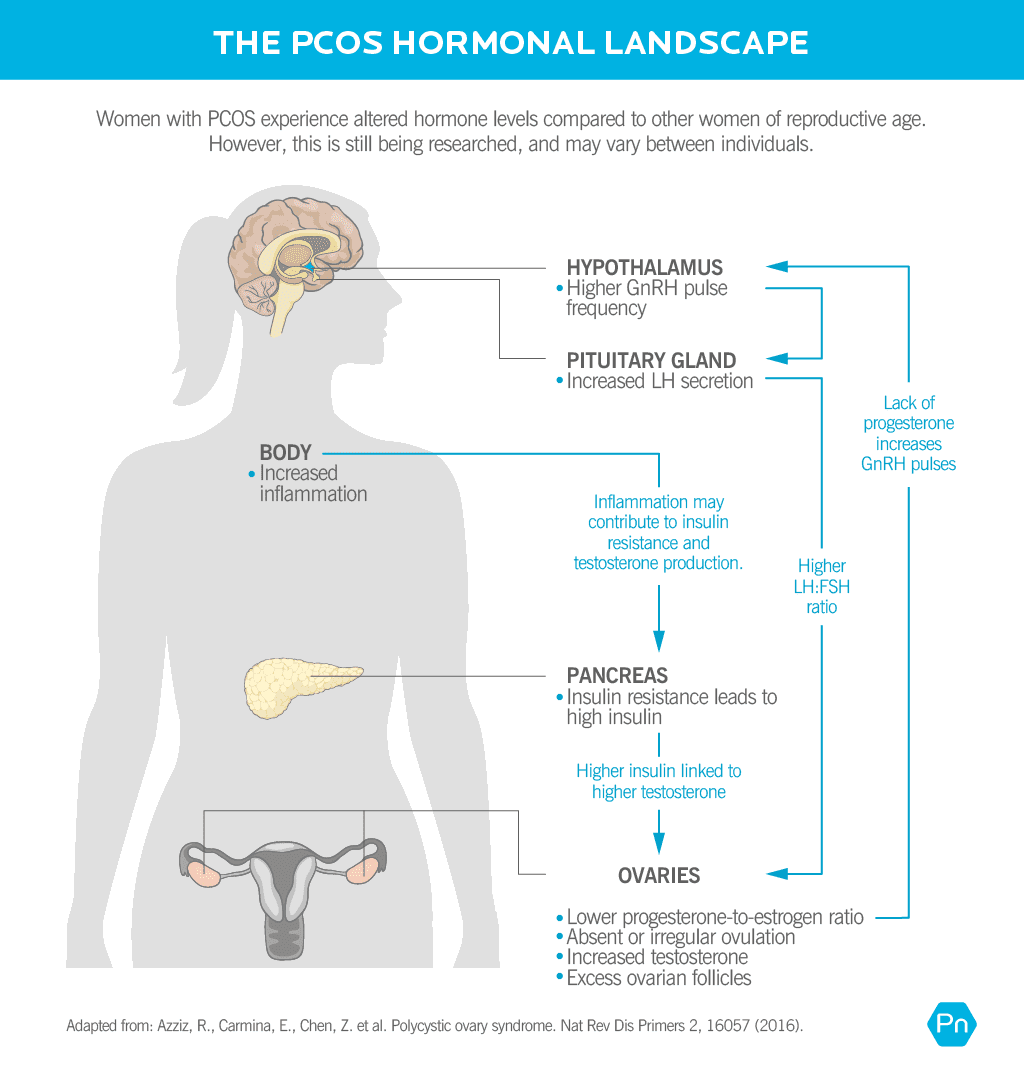
In a normal menstrual cycle, the hypothalamus releases a hormone called gonadotropin-releasing hormone (GnRH) in regular pulses, triggering the pituitary gland to release two other hormones:
- follicle-stimulating hormone (FSH)
- luteinizing hormone (LH)
FSH and LH travel to the ovary, prompting the release of estrogens, androgens, and progesterones. The right ratio of these hormones stimulates ovulation, or the release of an egg.
In PCOS, the hypothalamus releases GnRH at a higher frequency.
Faster and longer GnRH pulses disrupt the normal ratio of LH and FSH. Many (though not all) women with PCOS will have higher levels of LH. More LH triggers the production of more androgens—like testosterone—and inhibits ovulation.
High insulin—a common feature of PCOS—can further contribute to androgen production as well as decrease another hormone called sex hormone binding globulin (SHBG), which can lead to even higher amounts of circulating free testosterone.
Women may also have dysregulated thyroid and adrenal function.
Just like the ovaries, the thyroid and adrenal glands depend on normal hypothalamic and pituitary function.
It’s this hormonal circus that causes the grab-bag of symptoms that appear across various systems of the body.
What causes PCOS?
PCOS arises from a combination of four main influences.
Genetics
Multiple genes contribute to an increased risk of PCOS, although carrying a specific gene variant doesn’t guarantee you’ll exhibit symptoms.4, 5, 6
The fetal environment
If your mother has higher levels of testosterone during her pregnancy with you, your risk of developing PCOS goes up.7, 8
Childhood trauma
Chronic stress early in life can result in changes in the brain that alter hormone regulation, and increase the risk of many diseases, such as immune, metabolic, cardiovascular, and psychiatric disorders.9, 10
Women with PCOS are twice as likely to have experienced childhood trauma.11
Lifestyle habits
A sedentary lifestyle, poor nutrition, and obesity contribute to insulin resistance and excess inflammation.
This makes PCOS more likely, as well as worsens symptoms.
Getting adequate movement, good nutrition, and managing weight won’t cure you if you have PCOS, but they can improve symptoms, quality of life, and future health outcomes.12
Several environmental pollutants have been linked to PCOS, too.13
These include brominated diphenyl ethers, polychlorinated biphenyls, organochlorine pesticides, perfluorinated compounds, phthalates, and bisphenol A (BPA). Major hormone disruptors, these chemicals are found in air, water, soil, and food, as well as in household cleaning supplies, food containers, and beauty products.
PCOS symptoms
Hormonal imbalances produce a constellation of symptoms, which vary from person to person and range from very mild to severe.
 Menstrual irregularities: In addition to being longer or shorter than usual, periods may also be super heavy or very light.
Menstrual irregularities: In addition to being longer or shorter than usual, periods may also be super heavy or very light.
 Infertility / anovulation: High levels of androgens stop the release of an egg, inhibiting ovulation.
Infertility / anovulation: High levels of androgens stop the release of an egg, inhibiting ovulation.
 Ovarian “cysts” / follicles: Many—but not all—women with PCOS have a build-up of immature ovarian follicles (often erroneously called “cysts”).
Ovarian “cysts” / follicles: Many—but not all—women with PCOS have a build-up of immature ovarian follicles (often erroneously called “cysts”).
 Changes in hair growth: High androgen levels can cause coarse hair to develop on the face, chest, belly, or back, a symptom known as hirsutism. Meanwhile, hair at the crown and frontline of the head may begin to thin.
Changes in hair growth: High androgen levels can cause coarse hair to develop on the face, chest, belly, or back, a symptom known as hirsutism. Meanwhile, hair at the crown and frontline of the head may begin to thin.
 Weight gain and / or stubborn weight loss: Weight can stick around like a stubborn barnacle, possibly due to the combination of high androgens, high blood sugar and insulin, unregulated inflammation, and/or a sluggish thyroid.
Weight gain and / or stubborn weight loss: Weight can stick around like a stubborn barnacle, possibly due to the combination of high androgens, high blood sugar and insulin, unregulated inflammation, and/or a sluggish thyroid.
 Acne: High androgen and insulin levels may contribute to oily skin and stubborn acne—especially around the chin, but also on other parts of the face, back, or chest. Painful, longer-lasting cysts can also appear around the underarms, under the breasts, or around the groin, a condition called hidradenitis suppurativa or acne inversa.
Acne: High androgen and insulin levels may contribute to oily skin and stubborn acne—especially around the chin, but also on other parts of the face, back, or chest. Painful, longer-lasting cysts can also appear around the underarms, under the breasts, or around the groin, a condition called hidradenitis suppurativa or acne inversa.
 Dark skin patches: Also known as acanthosis nigricans, high insulin levels can cause darkened, thickened, velvety skin in the creases of the body, particularly around the armpits, neck, and groin.
Dark skin patches: Also known as acanthosis nigricans, high insulin levels can cause darkened, thickened, velvety skin in the creases of the body, particularly around the armpits, neck, and groin.
 Low energy and carb cravings: Some women with PCOS have a reduced ability to tolerate processed carbs. Translation: 15 minutes after you’ve eaten that scone, you’ve dozed off and your face is molding to your keyboard.
Low energy and carb cravings: Some women with PCOS have a reduced ability to tolerate processed carbs. Translation: 15 minutes after you’ve eaten that scone, you’ve dozed off and your face is molding to your keyboard.
 Increased risk of diabetes: Compared to the general population, women with unmanaged PCOS are more than four times more likely to develop type 2 diabetes, and nearly three times more likely to develop gestational diabetes.14
Increased risk of diabetes: Compared to the general population, women with unmanaged PCOS are more than four times more likely to develop type 2 diabetes, and nearly three times more likely to develop gestational diabetes.14
 Blood lipid imbalances: High blood sugar and insulin can contribute to low levels of high-density lipoprotein (the “good” cholesterol), high triglycerides, and a higher risk of cardiovascular disease.
Blood lipid imbalances: High blood sugar and insulin can contribute to low levels of high-density lipoprotein (the “good” cholesterol), high triglycerides, and a higher risk of cardiovascular disease.
 Sleep issues: PCOS is linked to sleep apnea, which is when breathing periodically stops during sleep.15
Sleep issues: PCOS is linked to sleep apnea, which is when breathing periodically stops during sleep.15
 Mood swings, anxiety, and depression: PCOS can increase the likelihood of mood swings, anxiety, and depression.16 Because many women with PCOS struggle with their weight, they’re also at an increased risk of disordered eating.
Mood swings, anxiety, and depression: PCOS can increase the likelihood of mood swings, anxiety, and depression.16 Because many women with PCOS struggle with their weight, they’re also at an increased risk of disordered eating.
Both the visible and invisible symptoms of PCOS can be incredibly distressing, taking a toll on self-esteem.
Thankfully, there’s help.
PCOS and Hashimoto’s thyroiditis.
Women with Hashimoto’s thyroiditis—an autoimmune condition of the thyroid—are more than three times as likely to have PCOS, compared to the regular population.17, 18
Why are the two related? It’s still unclear.
What we do know:
- Both PCOS and Hashimoto’s thyroiditis have a strong genetic component. A handful of genes (FBN, GNRHR and CYP1B1) have been linked to both, although researchers aren’t confident these genes fully explain their association.19
- Women with PCOS have a higher estrogen to progesterone ratio, which can increase immune activity. This is bad news for autoimmune conditions like Hashimoto’s, which are characterized by an already overactive immune system.
- Women with PCOS may have less gut microbiome diversity.20, 21 This can further compromise the immune system.
This landscape in is like adding gasoline to an autoimmune fire, increasing the likelihood of Hashimoto’s.22
PCOS treatment
Out there on the Internet, you’ll find PCOS treatment plans that list dozens of “never eat” foods and sweat-til-you-drop fitness regimens.
You won’t find that here. In our experience of working with over 100,000 clients, we know one thing for sure: It takes a rare person to consistently stick to an extreme diet and fitness plan.
The good news: Most people see massive improvements with just three tiny and much-more-realistic lifestyle changes.
The PCOS diet: Be smart with carbs
To manage energy and blood sugar, you don’t need to (and probably shouldn’t) avoid carbs altogether, but some research shows that lower carb—and possibly low dairy—diets can be helpful.23
The advice
Put the focus on what to eat rather than what not to eat. Aim for about 10 grams of fiber and 20-30 grams of protein (roughly one palm-sized portion) per meal by building plates around these nutrient-rich foods.
- Lean proteins: meat and poultry, fish and shellfish, eggs, tofu and tempeh
- Colorful non-starchy vegetables: cruciferous veggies (think: broccoli, cabbage, and kale), lettuces, cucumber, celery, summer squash, tomatoes, mushrooms, peppers, and asparagus
- Low-sugar fruits: berries, apples, oranges, and plums
- Healthy fats: avocado, olives, nuts and seeds, and oils (olive and coconut)
With the above taking up the most space, fill out your plate with smaller amounts of dairy, starchy veggies, or whole grains.
For help making more nutritious food choices, check out this visual guide: ‘What should I eat?!’
And for more specific nutrition recommendations tailored to your body, lifestyle, and goals—including portion suggestions for the above food groups—see: The Precision Nutrition Calculator.
Are there any supplements that help PCOS?
Below is a list of the most effective, evidence-based supplements used to manage PCOS.
If you’re a coach, encourage your client to first talk to their doctor.
| Nutrient | Mechanism of action | Level of evidence | Recommended dose |
|---|---|---|---|
| Inositol | Helps regulate hormone levels and menstrual cycles, as well as improve insulin sensitivity, egg quality, and fertility. 24, 25, 26 | Very high | Two forms are most effective: Myo-inositol (4,000 mg/day) and D-chiro-inositol (100 mg/day) |
| Zinc | Zinc deficiency is more common in women with PCOS,27 and supplementation may regulate hair growth and improve skin quality.28 | Moderate | 30-50 mg/day for 8 weeks, with a meal (can cause nausea on an empty stomach) |
| Vitamin D | Plays a role in ovarian follicle development and progesterone production, both important for maintaining a healthy menstrual cycle and fertility.29 | Moderate | If a blood test confirms a deficiency, 1,000-2,000 IU/day can help normalize levels |
| Magnesium | Helps regulate blood sugar, estrogen, and progesterone production, and supports the nervous system. | Moderate | 200-400 mg/day |
| Chromium | Improves insulin sensitivity, and may help lower high blood sugar.30 | Moderate | 200-1,000 mcg/day (at the higher range, separate doses into two or more) |
PCOS exercise: Find joyful movement
Most beings benefit from regular movement. (Even pet hamsters are happier with a running wheel in their cage.)
In women with PCOS, exercise can:
- Improve ovulation and menstrual regularity31
- Improve insulin sensitivity
- Decrease androgens
- Decrease risk of cardiovascular disease
- Improve mental health32, 33
These benefits show up with or without additional changes in diet and regardless of weight changes. Meaning: Exercise is a superpowered tool.
The advice
Aim for at least 120 minutes of moderate-intensity exercise per week.34 That translates to about four 30-minute sessions, with (ideally) half of those sessions devoted to resistance training.
But start wherever you are.
 If you’re a regular gym go-er, keep at it. Resistance training may be especially beneficial, because it helps improve insulin sensitivity and the ratio of fat to lean mass.35 (Plus, lifting heavy things feels badass.)
If you’re a regular gym go-er, keep at it. Resistance training may be especially beneficial, because it helps improve insulin sensitivity and the ratio of fat to lean mass.35 (Plus, lifting heavy things feels badass.)
 If you get your movement mostly from errands, like carrying your groceries or walking to the bus stop, try adding a little more. Consider tracking your steps to get a baseline, then set a goal for a higher number. Or, add a once or twice weekly online or in-person exercise class or workout. (For a zero-equipment, 10-minute workout see: How to stay in shape when you’re busy.)
If you get your movement mostly from errands, like carrying your groceries or walking to the bus stop, try adding a little more. Consider tracking your steps to get a baseline, then set a goal for a higher number. Or, add a once or twice weekly online or in-person exercise class or workout. (For a zero-equipment, 10-minute workout see: How to stay in shape when you’re busy.)
 If the word “exercise” makes you want to wash your mouth with soap, just start anywhere. Even a five-minute walk or a dance party counts. (Wagging your finger and saying, “Nuh-uh,” doesn’t. Nice try though.)
If the word “exercise” makes you want to wash your mouth with soap, just start anywhere. Even a five-minute walk or a dance party counts. (Wagging your finger and saying, “Nuh-uh,” doesn’t. Nice try though.)
What’s most important: Find something that you actually enjoy doing, because you’ll be more likely to keep at it.
Choose the exercise flavor that most appeals to you. As you get comfortable and consistent with more movement, reassess, and add a little more if that aligns with your abilities and goals.
PCOS: Two different types?
Women with PCOS may have slightly different hormonal profiles (and symptoms) depending on whether they also have excess body fat. Recognizing the two subpopulations, experts use these terms36:
- The reproductive type (sometimes referred to as “lean PCOS”) tends to have a lower BMI and less insulin resistance, but higher luteinizing hormone (LH) and sex hormone binding globulin (SHBG).37
- The metabolic type tends to have a higher BMI, more glucose and insulin dysregulation, and lower LH and SHBG levels.
With the exception of weight loss, the lifestyle recommendations we suggest in this article still apply to both groups.
Stress management: Self-kindness is the new cool
With PCOS, it can be easy to fall into self-criticism and pessimistic thinking. That’s why, as you do your best to make healthy changes in your life, also bring in an abundance of self-compassion.
The advice
Pay attention to your thoughts, and when you notice yourself being unkind or overly critical, practice speaking to yourself as you would your best friend.
Acknowledge that your condition can be a real struggle sometimes.
And while it’s not your fault, it is your responsibility to take care of yourself in the best and kindest way you can.
It may help to remember that many other women are dealing with PCOS too. Joining a PCOS support group, or even just thinking about the other women who are “in this” with you can be helpful.
In addition to a self-compassionate mindset, make sure to prioritize those stress-busting basics.
 Get adequate sleep. Good sleep helps balance hormones and mood, makes it easier to regulate weight and appetite, and reduces the chance of “Tiredzilla” coming out to torment your friends and family. (For tips on how to improve sleep, read: The power of sleep.)
Get adequate sleep. Good sleep helps balance hormones and mood, makes it easier to regulate weight and appetite, and reduces the chance of “Tiredzilla” coming out to torment your friends and family. (For tips on how to improve sleep, read: The power of sleep.)
 Include daily stress-relieving activities. Meditation, walks in nature, time with loved ones, and creative hobbies are stress-busting superstars. For even more stress reducers, read: Feel like you’re failing at self care? 3 solutions that can actually help.
Include daily stress-relieving activities. Meditation, walks in nature, time with loved ones, and creative hobbies are stress-busting superstars. For even more stress reducers, read: Feel like you’re failing at self care? 3 solutions that can actually help.
 Be mindful of how you frame your PCOS story. Are you a helpless PCOS victim? Or, can PCOS be an opportunity to learn more about your health and take better care of yourself? Which story feels better? Which story motivates you to take empowering action?
Be mindful of how you frame your PCOS story. Are you a helpless PCOS victim? Or, can PCOS be an opportunity to learn more about your health and take better care of yourself? Which story feels better? Which story motivates you to take empowering action?
Of course, sometimes you can “do everything right” and still feel completely overwhelmed, maybe even hopeless. If that’s the case, reach out. Talk to a trusted loved one, your doctor, or a mental health professional.
Sometimes just knowing someone else is on your team can make the difference between “I’m in a black hole and I can’t get out” and “I see some light at the end of the tunnel.”
PCOS and weight loss
The truth is: It can be harder to lose weight when you have PCOS.
That’s one reason why it’s better to focus on the lifestyle habits we mentioned in the previous section. After all, what you eat and how you move has a bigger influence on your health and symptoms than does your weight on the scale.
In many cases, fat loss will happen as a natural side effect of better overall health. But if it doesn’t, you’ll still be eating, moving, feeling, and living better.
Advice for coaches
As a coach, it’s easy to feel out of your realm, wondering: “Am I really qualified to help someone with PCOS?”
And while coaches can’t diagnose or treat PCOS, you absolutely can support them—no special certifications required.
Keep in mind: Your client likely has access to healthcare experts who know the latest PCOS research and treatments.
What’s missing from your client’s life: Someone who can help them put what their doctor recommends into practice.
Most likely, their doctor will recommend strategies that are quite similar to the strategies you’ve already used with other clients: exercise, healthy eating, and stress relief, all of which can improve symptoms of PCOS tremendously.
Stay within your scope, and be the best cheerleader you can.
References
Click here to view the information sources referenced in this article.
If you’re a coach, or you want to be…
Learning how to coach clients, patients, friends, or family members through healthy eating and lifestyle changes—in a way that’s personalized for their unique body, preferences, and circumstances—is both an art and a science.
If you’d like to learn more about both, consider the Precision Nutrition Level 1 Certification.
The post PCOS: 3 evidence-based strategies that really work. appeared first on Precision Nutrition.

Nenhum comentário